Fillable Annual Physical Examination Form
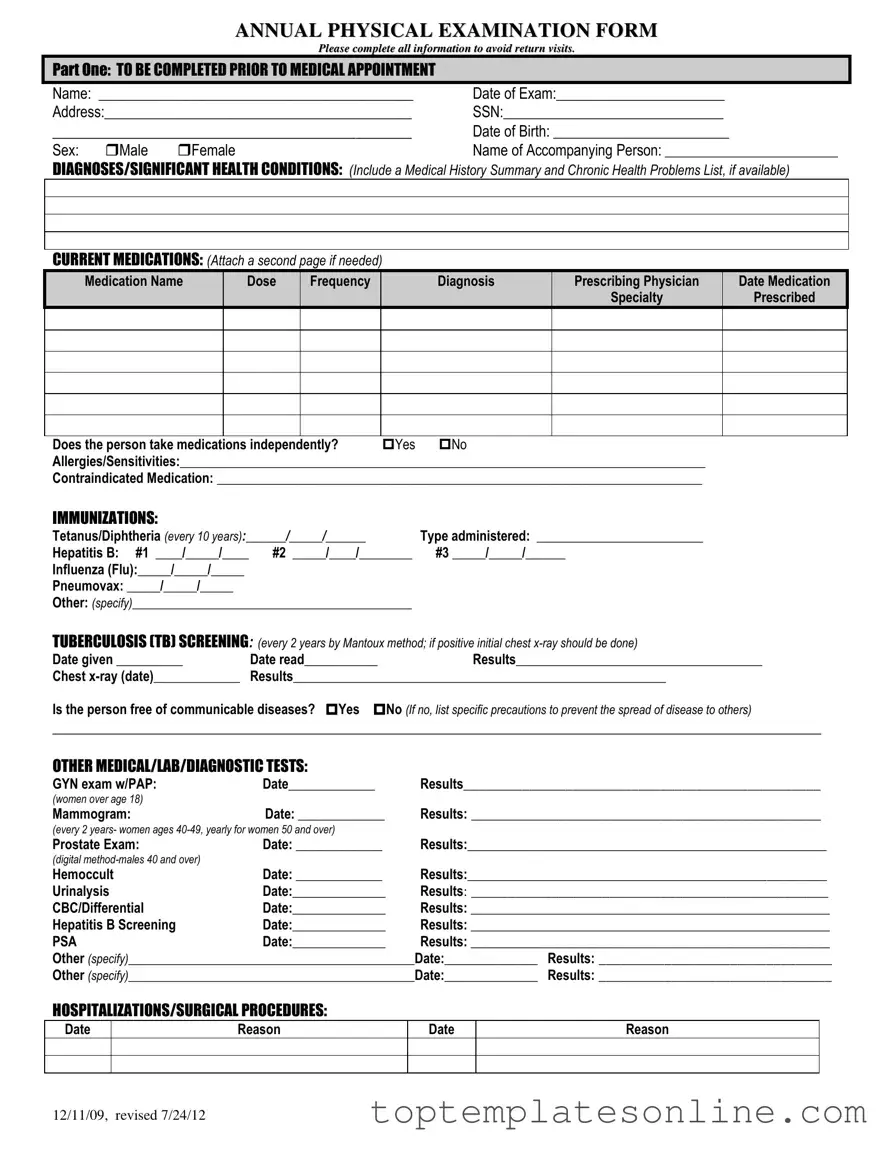
The Annual Physical Examination form is an essential tool designed to streamline the process of gathering vital health information before a medical appointment. It begins with a section for personal details, including the patient's name, date of birth, and contact information, ensuring that healthcare providers can easily identify and communicate with their patients. A comprehensive medical history is also crucial, as it invites patients to disclose any significant health conditions and current medications, including dosages and prescribing physicians. This section not only helps to avoid potential medication conflicts but also provides a clearer picture of the patient's overall health. Immunization records are meticulously documented, covering essential vaccinations like Tetanus, Hepatitis B, and Influenza, along with details of tuberculosis screening. The form further delves into any past hospitalizations or surgical procedures, offering insights into the patient's medical background. In the general physical examination section, healthcare professionals assess various bodily systems, recording blood pressure, pulse, and other vital signs, while also evaluating normal findings and any concerns that may arise. Finally, it allows for additional comments and recommendations tailored to the individual's health maintenance, ensuring a holistic approach to patient care. By completing this form thoroughly, patients can help facilitate a more productive and informative appointment, ultimately enhancing their healthcare experience.
Common PDF Templates
California Sdi - The EDD DE 2501 form is a claim for Disability Insurance benefits in California.
For landlords navigating the eviction process, utilizing a proper Notice to Quit is crucial. This document not only serves as a formal communication to the tenant but also ensures that the landlord is following legal protocols. To facilitate this process, landlords can access a comprehensive template at https://newyorkform.com/free-notice-to-quit-template, which can simplify the preparation of this important notice.
How to Make a Column Graph on Excel - Project Tracking: Implement this chart in project management to keep track of various elements and their status.
Declaration of Financial Support - The I-134 supports both humanitarian and family reunification efforts.
Common mistakes
-
Incomplete Personal Information: Failing to fill out all required personal details, such as the name, date of birth, or address, can lead to delays in processing. Ensure that every section is completed accurately.
-
Neglecting Medication Details: Omitting current medications or providing incorrect dosages and frequencies can result in significant health risks. It is essential to list all medications, including over-the-counter drugs, and to specify any allergies or sensitivities.
-
Inaccurate Health History: Not providing a complete medical history or failing to mention significant health conditions can affect the quality of care received. Include all relevant diagnoses and past hospitalizations.
-
Overlooking Immunization Records: Forgetting to update immunization dates or failing to mention recent vaccinations can lead to unnecessary tests or treatments. Always check that immunization information is current and accurate.
Guide to Writing Annual Physical Examination
Completing the Annual Physical Examination form accurately is essential for ensuring a smooth medical appointment. This form gathers vital information about your health history, current medications, and any significant health conditions. After filling it out, you will present it to your healthcare provider during your appointment.
- Part One: Prior to Your Appointment
- Write your full name in the designated space.
- Fill in the date of your exam.
- Provide your complete address.
- Enter your Social Security Number (SSN).
- Include your date of birth.
- Select your sex by marking the appropriate box (Male or Female).
- Write the name of the person accompanying you, if applicable.
- List any diagnoses or significant health conditions, including a summary of your medical history and chronic health problems if available.
- Document your current medications, including the name, dose, frequency, diagnosis, prescribing physician, and specialty. Attach a second page if necessary.
- Indicate whether you take medications independently by selecting Yes or No.
- List any allergies or sensitivities you have.
- Note any contraindicated medications.
- Complete the immunization section, providing dates and types of vaccines received.
- Fill out the tuberculosis screening section, including the date given and read, as well as the results.
- Answer whether you are free of communicable diseases and specify precautions if not.
- Document any other medical, lab, or diagnostic tests you have undergone, including the date and results.
- List any hospitalizations or surgical procedures with dates and reasons.
- Part Two: General Physical Examination
- Record your blood pressure, pulse, respirations, temperature, height, and weight.
- Evaluate each system listed, indicating normal findings with Yes or No and providing comments as necessary.
- Complete the vision and hearing screening sections, noting if further evaluation is recommended.
- Provide any additional comments regarding your medical history, medications, health maintenance recommendations, or special instructions.
- Note any limitations or restrictions for activities and whether you use adaptive equipment.
- Indicate if there has been a change in health status from the previous year.
- Answer whether this individual is recommended for ICF/ID level of care and if specialty consults are recommended.
- Document if a seizure disorder is present and the date of the last seizure.
- Print the name of your physician, have them sign, and provide the date, address, and phone number.
Documents used along the form
When preparing for an annual physical examination, several important forms and documents accompany the main examination form. Each of these documents serves a specific purpose, ensuring that healthcare providers have all the necessary information to deliver comprehensive care.
- Medical History Form: This document provides a detailed overview of the patient’s past medical issues, surgeries, and family health history. It helps physicians understand any hereditary conditions that may affect the patient’s health.
- Medication List: A current list of all medications the patient is taking, including prescriptions, over-the-counter drugs, and supplements. This information is crucial for preventing drug interactions and ensuring safe prescribing practices.
- Immunization Record: This record outlines the patient’s vaccination history, including dates and types of vaccines received. It assists healthcare providers in determining if any vaccinations are overdue or needed.
- Consent for Treatment Form: This document grants permission for healthcare providers to administer treatments and procedures. It ensures that patients are informed about the care they will receive and agree to it.
- Power of Attorney for a Child: A crucial document that allows a parent or legal guardian to designate another individual to make decisions on behalf of their child, especially in cases of temporary inability to care for them. For more information, visit Florida Forms.
- Referral Form: If a specialist consultation is needed, this form outlines the reason for the referral and provides pertinent medical information. It streamlines communication between primary care and specialty providers.
These documents, when completed accurately, contribute significantly to the quality of care received during an annual physical examination. They ensure that healthcare providers are well-informed and can make decisions that best support the patient’s health and well-being.