Attorney-Approved Do Not Resuscitate Order Form
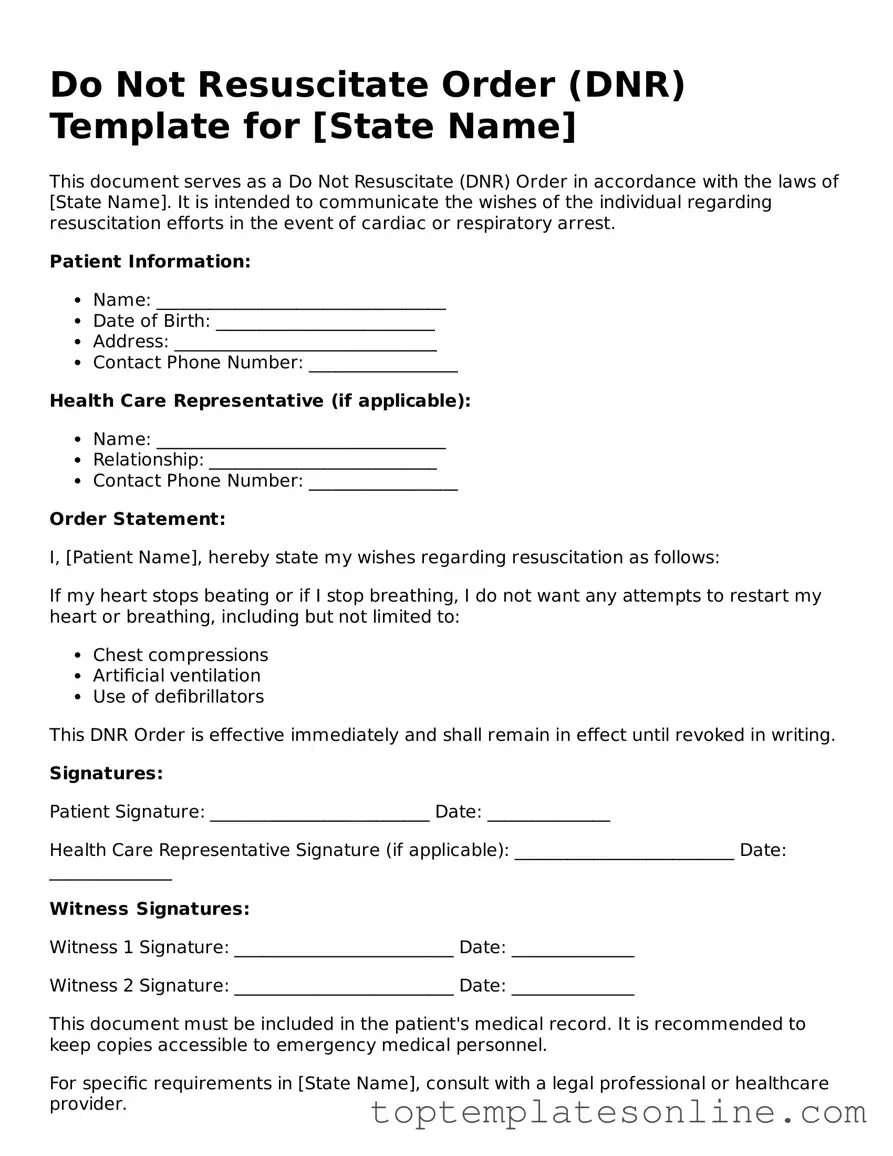
The Do Not Resuscitate (DNR) Order form serves as a crucial document in healthcare decision-making, particularly for individuals facing serious medical conditions. This form allows patients to communicate their wishes regarding resuscitation efforts in the event of cardiac arrest or respiratory failure. It is designed to ensure that healthcare providers respect the patient's preferences, which may stem from personal beliefs, medical conditions, or quality-of-life considerations. The DNR Order is typically completed in consultation with a healthcare professional, ensuring that the patient fully understands the implications of their decision. Additionally, it is important for the form to be easily accessible within the patient's medical records, as timely access can significantly impact the quality of care provided in emergencies. Understanding the nuances of the DNR Order is essential for both patients and families, as it plays a vital role in aligning medical interventions with individual values and wishes.
State-specific Information for Do Not Resuscitate Order Documents
Common Templates
How to Apply for Rent - Provide the address of your workplace, including city and state.
Open Ended Release Insurance - Document ensuring all parties have settled on the aspects of the accident.
For a smooth transaction, refer to this essential guide on the ATV Bill of Sale process, which lays out the vital steps for documenting your purchase or sale of an all-terrain vehicle.
Credit Application Template - Helps match businesses with suitable credit products.
Common mistakes
-
Not discussing the decision with family or loved ones: Many individuals fill out the Do Not Resuscitate (DNR) Order form without consulting their family members. This can lead to confusion or conflict during critical moments when decisions need to be made.
-
Failing to understand the implications: Some people do not fully grasp what a DNR order entails. It’s essential to recognize that this order means no resuscitation attempts will be made, which can be a difficult choice to make.
-
Not updating the form as circumstances change: Life situations can evolve. Failing to revisit and update the DNR order when health status or personal preferences change can lead to unintended consequences.
-
Inadequate signature or witness requirements: A DNR order must be properly signed and, in some states, witnessed. Omitting these steps can render the document invalid, negating its intended purpose.
-
Ignoring state-specific regulations: Each state has its own laws regarding DNR orders. Not adhering to these regulations can create legal issues or confusion for healthcare providers during emergencies.
Guide to Writing Do Not Resuscitate Order
Filling out a Do Not Resuscitate (DNR) Order form is an important step in ensuring that your healthcare preferences are honored in critical situations. This form communicates your wishes regarding resuscitation efforts in the event of a medical emergency. Below are the steps to complete the form accurately.
- Obtain the DNR Order form from your healthcare provider or download it from a reputable medical website.
- Read the instructions carefully to understand the requirements and implications of the form.
- Fill in your full name, date of birth, and any other identifying information as requested on the form.
- Specify the date on which you are completing the form.
- Indicate your wishes regarding resuscitation by checking the appropriate box or writing your preference in the designated section.
- Sign the form to validate your wishes. If required, have a witness sign as well.
- Provide the contact information of your healthcare proxy or power of attorney, if applicable.
- Review the completed form for accuracy and completeness.
- Make copies of the signed form for your records and distribute copies to your healthcare providers and family members.
Once the form is filled out and distributed, it is crucial to keep an open line of communication with your healthcare team and loved ones. This ensures that everyone is aware of your wishes and can act accordingly in the event of a medical emergency.
Documents used along the form
A Do Not Resuscitate (DNR) Order is a crucial document that outlines a person's wishes regarding medical treatment in the event of cardiac or respiratory arrest. In addition to the DNR, several other forms and documents may be relevant to ensure that an individual's healthcare preferences are respected. Below is a list of commonly associated documents.
- Advance Directive: This legal document allows individuals to specify their preferences for medical treatment in situations where they cannot communicate their wishes. It often includes decisions about life-sustaining measures and end-of-life care.
- Living Will: A type of advance directive, a living will outlines specific medical treatments an individual does or does not want in the event of a terminal illness or incapacitation. It serves to guide healthcare providers and family members.
- Healthcare Proxy: This document designates a trusted person to make medical decisions on behalf of an individual if they become unable to do so. The appointed proxy should be aware of the individual's values and healthcare preferences.
- Physician Orders for Life-Sustaining Treatment (POLST): This form translates a patient's wishes regarding life-sustaining treatments into medical orders. It is typically used for individuals with serious illnesses and ensures that their preferences are followed across different healthcare settings.
- Operating Agreement: For those establishing a limited liability company in New York, the essential Operating Agreement form resources provide the necessary framework to outline management structure and procedures.
- Patient Identification Wristband: While not a formal document, this wristband is often used in hospitals to communicate critical information about a patient's DNR status. It helps ensure that all healthcare providers are aware of the patient's wishes at a glance.
Understanding these documents can significantly impact the quality of care received during critical moments. By having these forms in place, individuals can ensure their healthcare preferences are honored and communicated effectively to medical personnel and loved ones.