Fillable Medication Administration Record Sheet Form
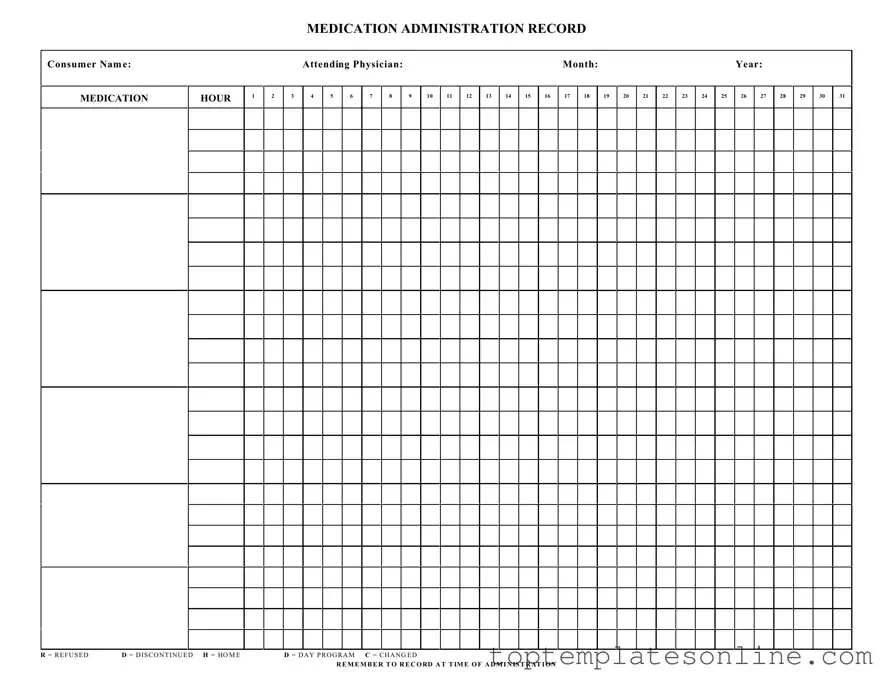
The Medication Administration Record Sheet (MARS) plays a crucial role in ensuring that patients receive their medications safely and effectively. This form is designed to track the administration of medications, detailing essential information such as the consumer's name, attending physician, and the specific month and year. Each hour of the day is clearly marked, allowing healthcare providers to document when medications are administered. The sheet includes designated spaces for recording various actions, such as refusal of medication (R), discontinuation (D), or changes in the medication regimen (C). Additionally, it emphasizes the importance of noting the exact time of administration, which is vital for maintaining accurate medication schedules. By using the MARS, healthcare professionals can enhance communication among team members and ensure that patients receive the correct dosages at the appropriate times, ultimately improving patient outcomes.
Common PDF Templates
Fake Vehicle Inspection Form - Inspect the vehicle's horn for functionality.
For individuals seeking to formalize rental agreements, understanding the New York Lease Agreement form is vital. This document ensures both landlords and tenants are aware of their obligations and rights throughout the rental period. You can learn more about this necessary documentation by visiting the important Lease Agreement details available online.
How Do You Become a Professional Cuddler - Choose between different cuddling options, from casual to serious.
How to Make a Column Graph on Excel - Educational Purposes: Students can use this chart to learn how to categorize information effectively.
Common mistakes
-
Incomplete Consumer Information: Failing to fill out the consumer's name can lead to confusion and errors in medication administration. Always ensure that the name is clearly written and legible.
-
Missing Dates: Omitting the month and year can create significant issues in tracking medication history. Always double-check that the date is clearly indicated at the top of the form.
-
Incorrect Medication Hours: Marking the wrong hour for medication administration can lead to missed doses or overdoses. Carefully verify the time before recording it on the sheet.
-
Improper Use of Abbreviations: Using abbreviations like R for refused or D for discontinued without proper context can cause misunderstandings. Always ensure that any abbreviations are clearly defined and understood by all staff members.
-
Failure to Record at Time of Administration: Not documenting the medication at the time it is given can result in inaccuracies. It's crucial to record the information immediately after administration to maintain an accurate medication history.
Guide to Writing Medication Administration Record Sheet
Filling out the Medication Administration Record Sheet is essential for tracking medication administration accurately. Follow these steps to ensure you complete the form correctly.
- Enter the Consumer Name: Write the full name of the consumer at the top of the form.
- Fill in the Attending Physician: Provide the name of the physician responsible for the consumer's care.
- Specify the Month and Year: Indicate the month and year for which you are recording medication administration.
- Record the Medication: In the designated column, write down the name of the medication being administered.
- Mark the Administration Hour: Use the appropriate hour column to indicate when the medication is given, from 1 to 31.
- Use Codes for Status: If the medication was refused, discontinued, or changed, mark the corresponding code (R, D, or C) in the appropriate box.
- Document at the Time of Administration: Ensure that you record each medication at the time it is administered for accurate tracking.
Documents used along the form
The Medication Administration Record Sheet (MARS) is a crucial document used in healthcare settings to track the administration of medications to patients. Several other forms and documents often accompany the MARS to ensure comprehensive medication management and patient safety. Below is a list of these documents, each serving a specific purpose in the medication administration process.
- Medication Order Form: This document is used by healthcare providers to prescribe medications for patients. It includes details such as the medication name, dosage, route of administration, and frequency.
- Patient Medication Profile: This profile provides a summary of all medications a patient is currently taking, including over-the-counter drugs and supplements. It helps healthcare providers avoid potential drug interactions.
- ATV Bill of Sale Form: For those engaging in off-road vehicle transactions, the necessary ATV Bill of Sale documentation ensures that ownership transfers are legally recognized.
- Medication Reconciliation Form: This form is utilized during transitions of care, such as hospital admissions or discharges. It ensures that all medications are accurately documented and reconciled between different healthcare settings.
- Side Effects and Adverse Reactions Log: This log is maintained to document any side effects or adverse reactions experienced by patients after medication administration. It is essential for monitoring patient safety.
- Consent for Medication Administration: This document is signed by patients or their legal guardians to provide consent for the administration of prescribed medications. It ensures that patients are informed about their treatment.
- Medication Incident Report: In the event of a medication error or near miss, this report is filled out to document the incident. It is crucial for analyzing the error and implementing corrective actions.
- Medication Disposal Record: This record is used to document the disposal of expired or unused medications. Proper disposal is important for environmental safety and compliance with regulations.
- Patient Education Materials: These materials provide patients with information about their medications, including usage instructions, potential side effects, and the importance of adherence to prescribed regimens.
Utilizing these forms in conjunction with the Medication Administration Record Sheet enhances the overall quality of care provided to patients. Each document plays a vital role in ensuring that medication management is conducted safely and effectively.