Blank Do Not Resuscitate Order Template for New York State
The New York Do Not Resuscitate (DNR) Order form is a critical document that allows individuals to express their wishes regarding medical treatment in emergency situations. This form is especially relevant for patients with terminal illnesses or those who wish to avoid aggressive life-saving measures, such as cardiopulmonary resuscitation (CPR). The DNR Order must be completed and signed by a physician, ensuring that it meets the legal requirements set forth by New York State law. In addition to the physician's signature, the form requires the patient's or their legal representative's consent, emphasizing the importance of clear communication about end-of-life care preferences. The DNR Order is designed to be easily accessible and recognizable, typically printed on bright yellow paper, which helps medical personnel identify it quickly in emergencies. Understanding the implications and proper use of this form is essential for patients and families navigating difficult healthcare decisions. By documenting their wishes, individuals can ensure that their preferences are honored during critical moments when they may be unable to communicate. This article will delve into the specifics of the New York DNR Order form, including its purpose, the completion process, and the rights of patients and their families.
Some Other State-specific Do Not Resuscitate Order Templates
How Old Do You Have to Be to Sign a Dnr - Advance planning, including a DNR, helps ensure that medical care aligns with personal values.
Do Not Resuscitate Order - This order reflects a conscious decision to refuse certain life-sustaining treatments in emergencies.
The New York Lease Agreement form is a crucial tool for both landlords and tenants, providing a clear framework for the rental relationship. By detailing all terms and conditions, it helps to prevent disputes and promotes a harmonious living arrangement. For those looking to draft or customize such a document, you can find a useful template at newyorkform.com/free-lease-agreement-template.
Dnr Comfort Care - This document is important for those facing terminal illness or advanced age who wish to avoid aggressive interventions.
Can a Medical Power of Attorney Override a Dnr - Patients can discuss their decision with family and medical professionals before completing the form.
Common mistakes
-
Incomplete Information: Failing to provide all required personal information, such as the patient's full name, date of birth, and address, can render the form invalid.
-
Improper Signatures: The form must be signed by the patient or their legal representative. Not obtaining the necessary signatures can lead to complications.
-
Missing Witness Signatures: In New York, the form requires the signatures of at least two witnesses. Omitting these can invalidate the order.
-
Failure to Date the Form: Not including the date of signing can create confusion about the order's validity and intent.
-
Using Outdated Forms: Submitting an outdated version of the Do Not Resuscitate Order form can lead to legal issues. Always ensure the latest version is used.
-
Not Discussing with Healthcare Providers: Failing to communicate the decision with healthcare providers may lead to misunderstandings during critical situations.
-
Neglecting to Inform Family Members: Not informing family members about the existence of the order can cause distress and confusion during emergencies.
-
Inadequate Storage: Keeping the form in an inaccessible location can hinder its use when needed. It should be stored where it can be easily found by healthcare personnel.
-
Misunderstanding the Implications: Not fully understanding the implications of a Do Not Resuscitate Order can lead to unintended consequences for the patient and their family.
-
Failure to Review Periodically: Not reviewing the order regularly can result in outdated wishes not being honored. It is important to ensure the order reflects current preferences.
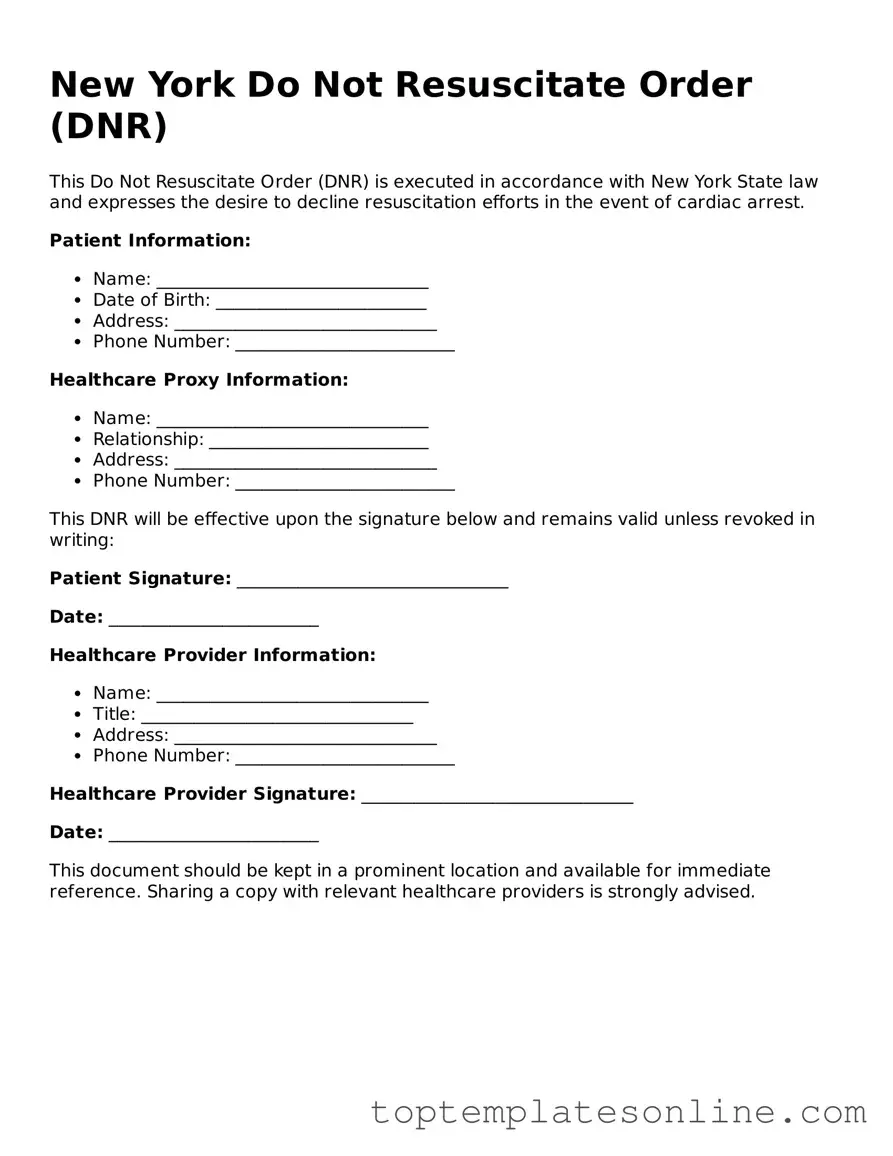
Guide to Writing New York Do Not Resuscitate Order
Completing the New York Do Not Resuscitate Order form is an important step for individuals who wish to communicate their healthcare preferences. Follow these steps carefully to ensure the form is filled out correctly.
- Obtain the New York Do Not Resuscitate Order form. This can be found online or through healthcare providers.
- Fill in the patient's full name at the top of the form.
- Provide the patient's date of birth.
- Indicate the patient's address, including city, state, and zip code.
- Check the box that confirms the patient understands the implications of the Do Not Resuscitate Order.
- Have the patient or their legal representative sign and date the form.
- Include the name and contact information of the physician who is completing the order.
- Ensure that the physician signs and dates the form as well.
- Make copies of the completed form for the patient, their family, and the healthcare provider.
After completing the form, it is important to distribute copies to all relevant parties. This ensures that healthcare providers are aware of the patient's wishes in case of a medical emergency.
Documents used along the form
The New York Do Not Resuscitate Order (DNR) form is an important document for individuals who wish to make their end-of-life preferences known. Along with the DNR form, several other documents can provide clarity and support for medical decisions. Here are five common forms that are often used in conjunction with the DNR:
- Health Care Proxy: This document allows an individual to appoint someone to make medical decisions on their behalf if they are unable to do so. It ensures that personal wishes are respected even when the individual cannot communicate them.
- Living Will: A living will outlines a person's preferences regarding medical treatment in situations where they cannot express their wishes. It typically addresses issues such as life support and other life-sustaining treatments.
- Physician Orders for Life-Sustaining Treatment (POLST): POLST is a medical order that details a patient’s preferences for treatments, including resuscitation and other interventions. It is designed to be honored by healthcare providers across various settings.
- Power of Attorney for a Child: This document ensures that a designated individual can make decisions for your child during your absence, and you can find more information at Florida Forms.
- Advance Directive: This is a broader term that encompasses both the living will and health care proxy. It serves as a guide for healthcare providers and family members regarding a person's healthcare preferences.
- Do Not Intubate (DNI) Order: Similar to a DNR, a DNI order specifies that a patient does not wish to be intubated or placed on a ventilator. This document is crucial for patients who want to avoid invasive respiratory support.
Having these documents in place can help ensure that medical care aligns with personal wishes. It is essential to discuss these forms with family members and healthcare providers to ensure everyone understands the intentions behind them.