Blank Do Not Resuscitate Order Template for North Carolina State
In North Carolina, the Do Not Resuscitate (DNR) Order form serves as a crucial document for individuals who wish to express their preferences regarding medical treatment in the event of a life-threatening emergency. This form is particularly significant for those with serious health conditions or advanced age, as it allows them to communicate their desire to forgo resuscitation efforts, such as CPR, should their heart or breathing stop. The DNR Order must be completed and signed by a qualified healthcare provider, ensuring that it meets the state's legal requirements. Additionally, the form requires the signature of the patient or their legal representative, which emphasizes the importance of informed consent in medical decision-making. Understanding how to properly complete and utilize this form can provide peace of mind for patients and their families, allowing them to focus on quality of life rather than the stress of emergency medical interventions. By having a DNR Order in place, individuals can ensure their healthcare wishes are respected, even in critical situations.
Some Other State-specific Do Not Resuscitate Order Templates
Do Not Resuscitate Form Georgia - A DNR does not limit access to palliative care or pain management for patients.
When considering your legal documents, understanding the importance of a properly executed Durable Power of Attorney form guide can provide peace of mind. This form empowers an individual to make crucial decisions on your behalf, particularly during times of incapacity, ensuring that your preferences are respected.
How Old Do You Have to Be to Get a Dnr - This decision can reflect an individual’s beliefs and desires about quality of life.
Do Not Resuscitate Order - A DNR can help ensure that patients receive only the level of care they desire during critical moments.
Common mistakes
-
Not Understanding the Purpose: Many individuals fill out the Do Not Resuscitate (DNR) Order form without fully grasping its implications. It is crucial to understand that this document indicates a person's wish to not receive CPR or advanced life support in case of cardiac or respiratory arrest.
-
Inaccurate Personal Information: Filling in incorrect personal details, such as name, date of birth, or medical record number, can lead to confusion. Ensure that all information is accurate and up-to-date to avoid issues during emergencies.
-
Not Discussing with Healthcare Providers: Some individuals neglect to consult with their doctors before completing the form. It is important to have a conversation about the decision and understand the medical context behind it.
-
Failure to Sign and Date: A common oversight is forgetting to sign and date the form. Without a signature, the document may not be considered valid, potentially leading to unwanted resuscitation efforts.
-
Not Informing Family Members: After completing the DNR Order, some people fail to inform their family members about their decision. Open communication can prevent confusion and ensure that everyone is aware of the individual’s wishes.
-
Using an Outdated Version: Individuals may inadvertently use an outdated version of the DNR form. Always check for the most current version to ensure compliance with state regulations.
-
Not Reviewing Regularly: Life circumstances can change, and so can medical preferences. Failing to review and update the DNR Order periodically can lead to situations where the document no longer reflects the individual’s wishes.
-
Neglecting to Keep Copies Accessible: After completing the form, some individuals do not make copies or fail to keep them in easily accessible locations. It is vital to have copies available for healthcare providers and family members.
-
Assuming It Is Automatically Recognized: Just because a DNR form is filled out does not mean it will be automatically honored. Individuals should ensure that healthcare providers are aware of the order and have access to the document when needed.
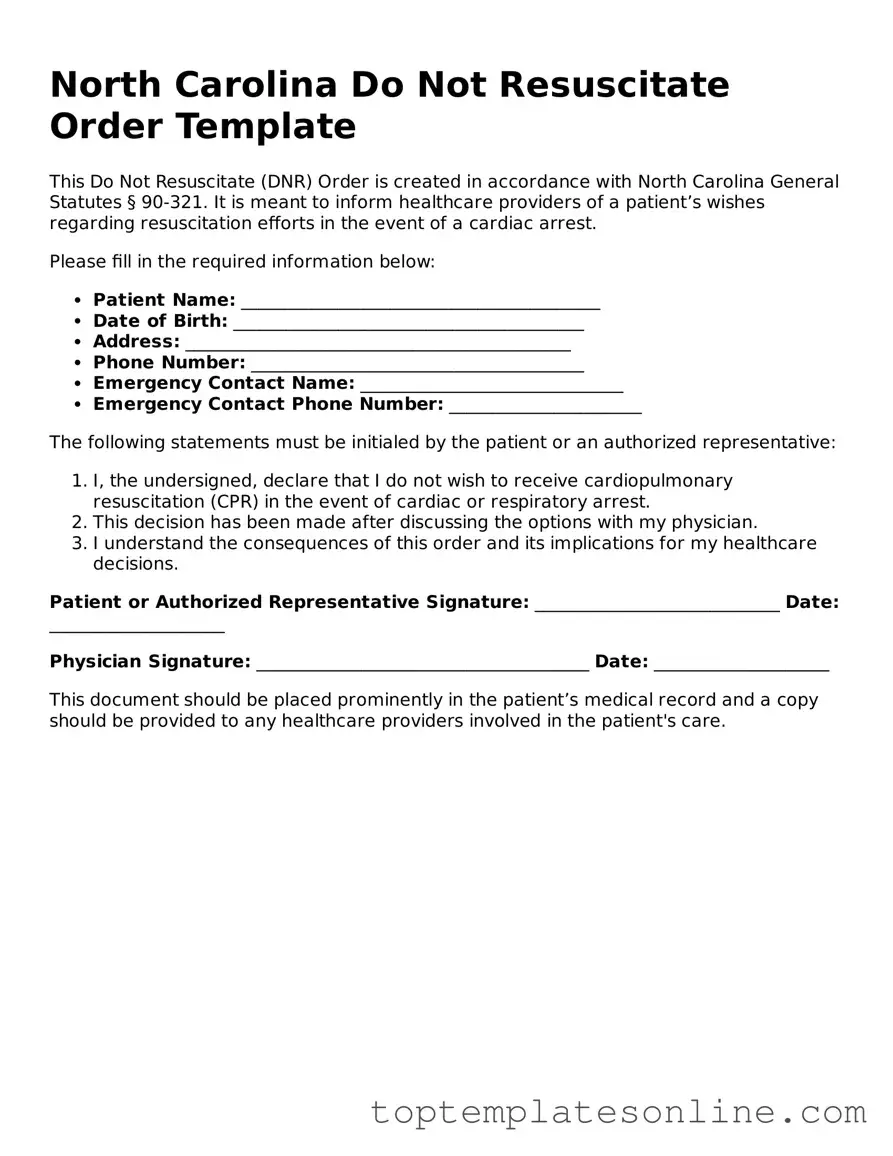
Guide to Writing North Carolina Do Not Resuscitate Order
Completing the North Carolina Do Not Resuscitate Order form is a straightforward process. After filling out the form, ensure that it is signed and dated by the appropriate parties. Keep a copy for your records and provide copies to your healthcare providers.
- Obtain the North Carolina Do Not Resuscitate Order form. You can find it online or request it from your healthcare provider.
- Fill in the patient's full name and date of birth at the top of the form.
- Indicate the patient's medical condition that warrants the DNR order.
- Specify the name of the healthcare provider who is authorizing the DNR order.
- Have the healthcare provider sign and date the form.
- Ensure that the patient or their legal representative also signs the form, if applicable.
- Make copies of the completed form for your records and for your healthcare providers.
Documents used along the form
In North Carolina, the Do Not Resuscitate (DNR) Order form is a critical document for individuals who wish to express their preferences regarding resuscitation efforts in the event of a medical emergency. Alongside this form, several other documents are commonly utilized to ensure that a person's healthcare wishes are honored. Here is a list of five important forms and documents that may accompany a DNR Order.
- Advance Directive: This document outlines a person's healthcare preferences in the event they become unable to communicate their wishes. It can include instructions about medical treatment, end-of-life care, and appointing a healthcare proxy.
- Healthcare Power of Attorney: This legal form allows an individual to designate someone else to make healthcare decisions on their behalf if they are incapacitated. This person, known as the agent, can advocate for the individual's wishes and preferences regarding treatment.
- Power of Attorney for a Child: This important legal document allows a parent or guardian to designate another individual to make decisions for their child in the parent's absence, ensuring that the child's needs are met. For more information, you can refer to Florida Forms.
- Living Will: A living will is a specific type of advance directive that details a person's wishes regarding life-sustaining treatments. It typically addresses situations where the individual is terminally ill or in a persistent vegetative state.
- Physician Orders for Scope of Treatment (POST): This document translates a patient's preferences into actionable medical orders. It is designed for individuals with serious health conditions and includes specific instructions about treatments and interventions.
- Do Not Hospitalize (DNH) Order: This order is used for patients who wish to avoid hospitalization, particularly in end-of-life scenarios. It specifies that the individual should receive care in a home or palliative setting instead of being admitted to a hospital.
Each of these documents plays a vital role in ensuring that an individual's healthcare wishes are respected and followed. By having these forms in place, individuals can communicate their preferences clearly to healthcare providers and loved ones, helping to avoid confusion during critical moments.