Fillable Prescription Label Form
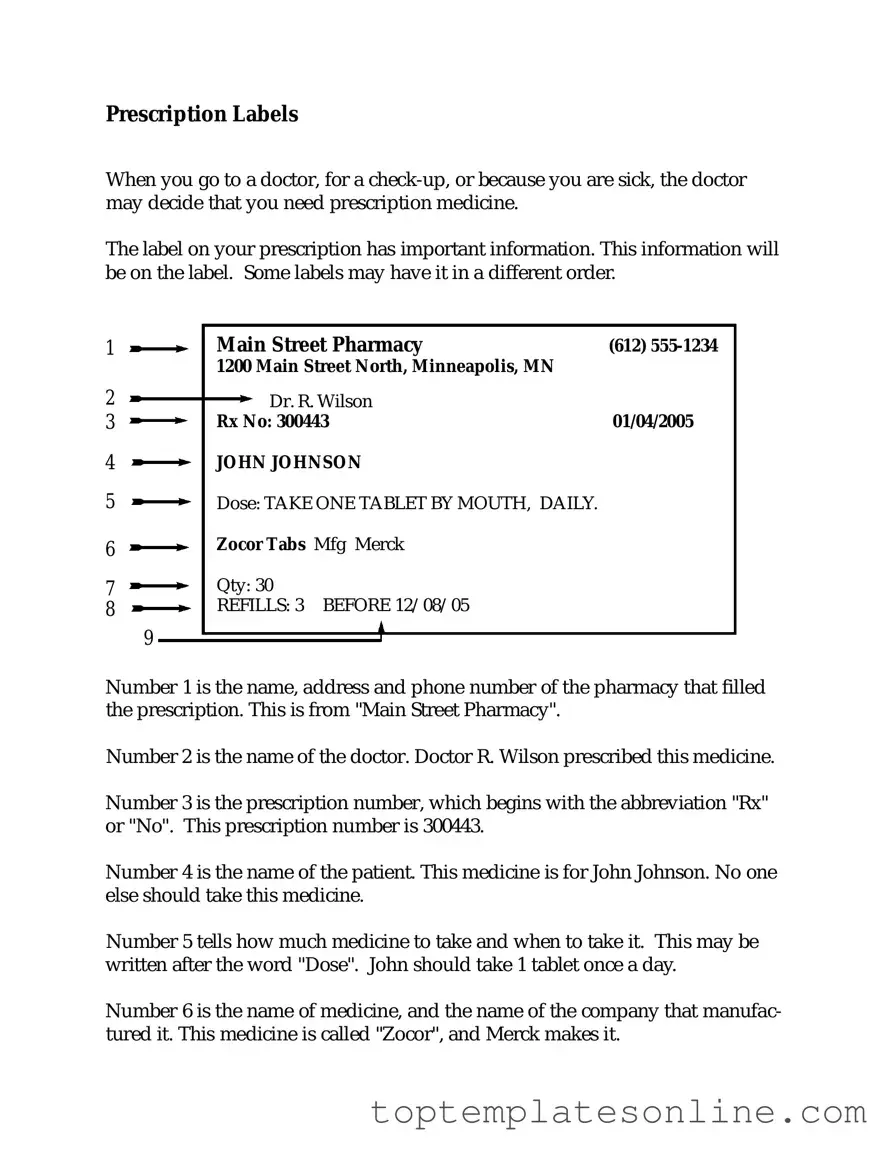
The Prescription Label form plays a crucial role in ensuring that patients receive their medications safely and effectively. This form includes essential information such as the patient's name, the prescribing physician's details, and the medication's name and dosage. Additionally, it outlines the directions for use, potential side effects, and any special instructions that may be necessary for the patient's health. The clarity and accuracy of this information are vital, as they help prevent medication errors and promote adherence to treatment plans. Understanding the components of the Prescription Label form can empower patients to take an active role in their healthcare, fostering better communication with their healthcare providers. This article will explore the significance of each aspect of the form, highlighting how it contributes to patient safety and effective medication management.
Common PDF Templates
Goodwill Receipt Online - Lists items donated to help with tax reporting.
The Florida Trailer Bill of Sale form is essential for anyone looking to purchase or sell a trailer in Florida, as it ensures that all necessary information regarding the transaction is documented. To simplify the process, you can access the form directly at https://floridaforms.net/blank-trailer-bill-of-sale-form/, making sure you have everything you need for a legitimate transfer of ownership.
View P60 Online - The information in the P45 is vital for ensuring correct tax deductions in the future.
Common mistakes
-
Incorrect Patient Information: Many individuals mistakenly enter the wrong name or date of birth. This can lead to confusion and delays in receiving the correct medication.
-
Missing Dosage Instructions: Some people forget to include specific dosage instructions. Without clear guidance, it may be unclear how much medication to take and how often.
-
Omitting Allergies: Failing to list known allergies can pose serious health risks. It is crucial to communicate any allergies to ensure safe medication use.
-
Inaccurate Medication Details: Individuals sometimes provide incorrect information about the medication itself, such as the name or strength. This can lead to receiving the wrong prescription altogether.
Guide to Writing Prescription Label
Completing the Prescription Label form is an important step in ensuring that your medication is accurately dispensed. Follow the steps below to fill out the form correctly. Take your time, and double-check your entries for accuracy.
- Start by entering the patient's full name in the designated field.
- Next, provide the patient's date of birth. This helps to confirm their identity.
- Fill in the name of the medication as it appears on the prescription.
- Indicate the dosage of the medication. This is usually specified in milligrams or another unit.
- Enter the quantity of medication prescribed. This is how many units the patient should receive.
- Specify the directions for use. Include how often the patient should take the medication and any specific instructions.
- Finally, sign and date the form at the bottom to validate it.
Documents used along the form
When it comes to managing prescriptions, several key forms and documents work alongside the Prescription Label form to ensure clarity and compliance in medication management. Each of these documents serves a unique purpose, helping both healthcare providers and patients navigate the complexities of prescriptions effectively.
- Prescription Order Form: This document is the initial request from a healthcare provider to a pharmacy, detailing the medication prescribed, dosage, and instructions for use.
- Non-disclosure Agreement (NDA): A Florida Non-disclosure Agreement (NDA) is a legally binding contract designed to protect sensitive information shared between parties. By signing this agreement, individuals or businesses commit to keeping confidential information private, ensuring that proprietary details remain secure. For further details, consult Florida Forms.
- Medication Administration Record (MAR): Used primarily in healthcare settings, this form tracks the administration of medications to patients, ensuring that they receive the correct doses at the right times.
- Patient Information Leaflet: Accompanying the medication, this leaflet provides essential information about the drug, including potential side effects, interactions, and usage guidelines.
- Drug Utilization Review (DUR): This document assesses the appropriateness of prescribed medications, aiming to prevent potential drug interactions and ensure patient safety.
- Prior Authorization Form: In some cases, insurance companies require this form to approve coverage for certain medications, necessitating additional information from the prescribing physician.
- Refill Authorization Form: This form is used when a patient needs to request a refill for their prescription, ensuring that the pharmacy has the necessary information to process the request.
- Controlled Substance Prescription Form: For medications classified as controlled substances, this specialized form is required to comply with federal regulations, detailing the specific medication and patient information.
Understanding these forms and their purposes can greatly enhance the prescription process for both patients and healthcare providers. By utilizing these documents effectively, everyone involved can contribute to safer and more efficient medication management.