Fillable Tb Test Form
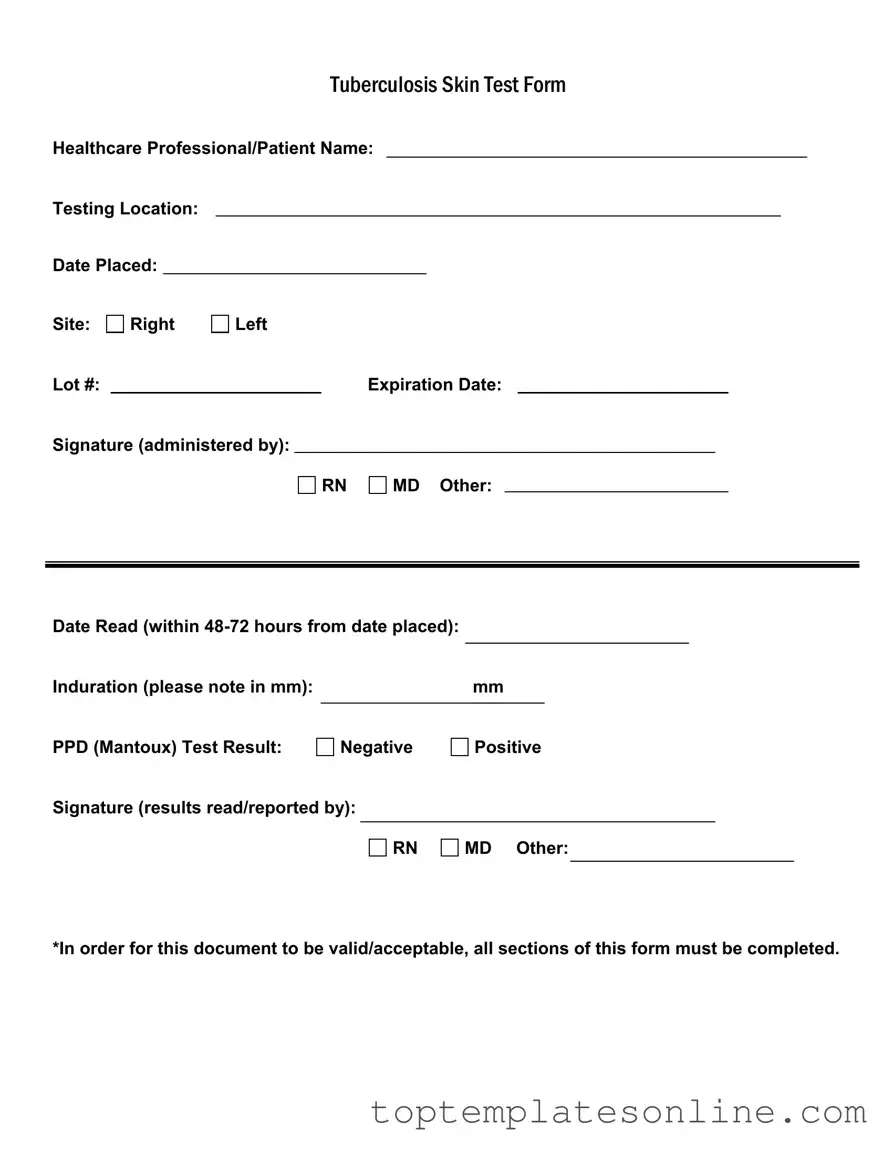
The Tuberculosis (TB) Skin Test Form is an essential document used in the healthcare setting to record critical information regarding TB testing. This form captures key details, starting with the names of both the healthcare professional administering the test and the patient receiving it. It includes the testing location and the date when the test was placed, ensuring that all relevant timelines are documented accurately. Additionally, the form specifies the site of the test on the patient's body, allowing for precise tracking of the procedure. Each form features a unique lot number and an expiration date for the testing material, which are crucial for maintaining the integrity of the test results. The signature of the administering professional, whether a registered nurse (RN), medical doctor (MD), or another qualified individual, is required to validate the test. Following the placement of the test, the form also prompts for the date the results are read, which must occur within 48 to 72 hours. Induration, measured in millimeters, is noted to assess the body's reaction to the test. Finally, the form concludes with the PPD (Mantoux) test result, which can be either negative or positive, and requires another signature to confirm that the results have been accurately read and reported. For the document to be considered valid and acceptable, it is imperative that all sections are completed thoroughly.
Common PDF Templates
Gift Certificate Template Free Editable - Our gift certificate allows for a personalized shopping experience.
Army Pubs Da 31 - The leave address must include complete contact details.
Utilizing the New York Boat Bill of Sale form is crucial for a smooth ownership transfer process, and for those looking for a reliable template, NY Templates offers an excellent resource that ensures all necessary details are included, keeping both buyers and sellers informed and compliant with state regulations.
T-47 - This form helps establish clear title to the property.
Common mistakes
-
Incomplete Information: One common mistake is not filling out all sections of the form. Each part, including the healthcare professional's name, testing location, and lot number, must be completed. Leaving any section blank can lead to delays or issues with processing the test results.
-
Incorrect Dates: It's crucial to accurately record the date the test was placed and the date it was read. Failing to do so can create confusion. The test results must be read within 48-72 hours of placement, so ensure these dates are correct.
-
Missing Signatures: Both the person administering the test and the individual reading the results must sign the form. Omitting these signatures can render the document invalid. Always double-check that all required signatures are present before submitting.
-
Improper Measurement: When noting the induration in millimeters, accuracy is key. Misreporting the size of the induration can lead to incorrect interpretations of the test results. Take care to measure correctly and record the mm value clearly.
Guide to Writing Tb Test
After you fill out the TB Test form, it will be used to record important details about your test. Make sure all sections are complete for the document to be valid. Follow these steps to fill out the form accurately.
- Write the name of the healthcare professional or patient at the top of the form.
- Fill in the testing location where the TB test is being administered.
- Enter the date when the test was placed.
- Indicate the site of the test by marking either "Right" or "Left."
- Record the lot number of the test.
- Note the expiration date of the test.
- The healthcare professional administering the test should sign in the designated area.
- Enter the date when the results will be read (this should be within 48-72 hours from the date placed).
- Measure and note the induration in millimeters (mm).
- Mark the PPD (Mantoux) test result as either "Negative" or "Positive."
- The healthcare professional who reads the results should sign in the designated area.
Documents used along the form
When dealing with the TB Test form, several other documents may be needed to ensure proper health records and compliance. Here’s a list of common forms that often accompany the TB Test.
- Health History Form: This document collects information about a patient's past medical history, including previous illnesses, allergies, and medications. It helps healthcare providers understand the patient's overall health.
- Consent Form: Patients must sign this form to give permission for the TB test to be administered. It outlines the procedure and any potential risks involved.
- Immunization Records: This form provides a history of vaccinations received by the patient. It can be important to check for any previous vaccinations related to tuberculosis.
- Referral Form: If the patient needs to see a specialist or undergo further testing, this form is used to refer them to the appropriate healthcare provider.
- Follow-Up Appointment Schedule: This document outlines the next steps for the patient, including when to return for results or additional testing if necessary.
- Patient Education Materials: These materials provide information about tuberculosis, its transmission, and prevention. They help patients understand their health better.
- Power of Attorney Form: This document allows individuals to designate a trusted person to make decisions on their behalf in healthcare scenarios, ensuring that a representative can act according to their wishes when they are unable to do so. For more details, you can visit https://newyorkform.com/free-power-of-attorney-template.
- Lab Results Form: This form contains the results of the TB test and any other relevant lab tests. It is essential for tracking the patient's health status.
- Insurance Information Form: Patients may need to provide details about their insurance coverage. This form ensures that the test and any follow-up care are covered.
Having these documents ready can streamline the process and ensure that all necessary information is gathered. It helps both patients and healthcare providers manage tuberculosis testing effectively.