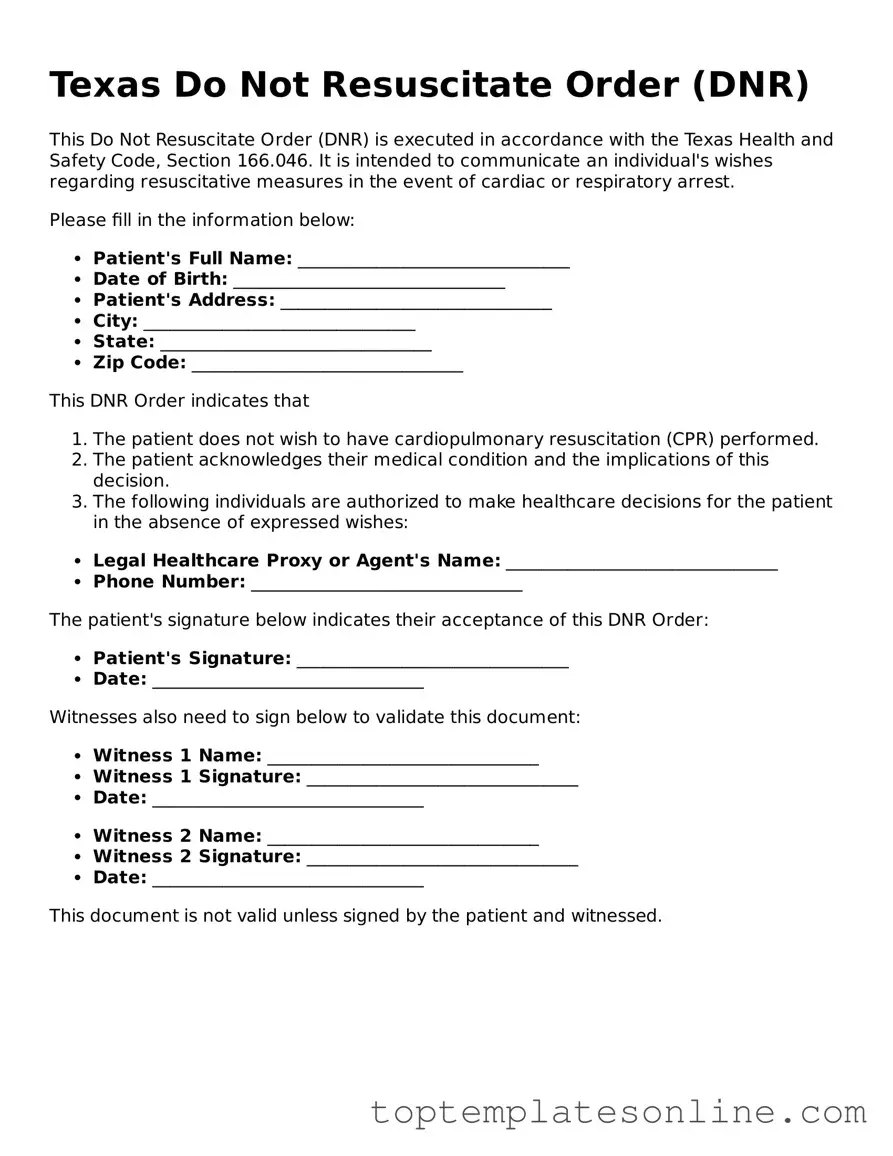
Blank Do Not Resuscitate Order Template for Texas State
The Texas Do Not Resuscitate Order (DNR) form is a crucial document that allows individuals to express their wishes regarding medical treatment in the event of a life-threatening situation. This form is designed for patients who prefer not to receive cardiopulmonary resuscitation (CPR) or other life-sustaining measures if their heart stops or they stop breathing. It is important for patients, families, and healthcare providers to understand the implications of this order. The DNR form must be completed and signed by the patient or their legally authorized representative, and it requires the signature of a physician to be valid. The document is intended to guide medical professionals in honoring the patient’s wishes during emergencies, ensuring that individuals receive care aligned with their personal values and preferences. In Texas, the DNR form is recognized across various healthcare settings, providing clarity and peace of mind for both patients and their loved ones. Understanding how to properly complete and implement this form can significantly impact end-of-life care decisions, making it essential for individuals to consider their options thoughtfully.
Some Other State-specific Do Not Resuscitate Order Templates
Can a Medical Power of Attorney Override a Dnr - A Do Not Resuscitate Order indicates that a person does not want CPR or advanced cardiac life support if their heart stops or they stop breathing.
For those looking to protect sensitive information, understanding the process is vital. A well-constructed Non-disclosure Agreement can serve as a cornerstone for maintaining confidentiality in business interactions. For more information, explore our insights on what a comprehensive Non-disclosure Agreement involves at comprehensive Non-disclosure Agreement considerations.
Do Not Resuscitate Form Georgia - The order reflects a choice to prioritize comfort over prolonging life at any cost.
Common mistakes
-
Not understanding the implications: Many individuals do not fully grasp what a Do Not Resuscitate (DNR) order entails. This can lead to confusion about when and how the order will be applied in medical situations.
-
Failing to communicate with healthcare providers: Some people neglect to discuss their wishes with their doctors or healthcare team. This can result in a lack of clarity about the patient's desires during emergencies.
-
Inaccurate or incomplete information: Errors in filling out personal details, such as name, date of birth, or signature, can invalidate the DNR order. It is crucial to ensure that all information is correct and complete.
-
Not reviewing or updating the order: Life circumstances can change, and so can a person's wishes regarding resuscitation. Failing to review and update the DNR order can lead to situations that do not align with the individual’s current preferences.
Guide to Writing Texas Do Not Resuscitate Order
Completing the Texas Do Not Resuscitate Order form is an important step in ensuring your medical wishes are respected. This form allows individuals to specify their preferences regarding resuscitation efforts in the event of a medical emergency. Follow these steps carefully to fill out the form accurately.
- Obtain a copy of the Texas Do Not Resuscitate Order form. You can find it online or request it from a healthcare provider.
- Read through the form to familiarize yourself with its sections and requirements.
- In the first section, provide your full name, date of birth, and any other identifying information requested.
- Designate a person to act as your representative, if desired. Include their name and contact information.
- Clearly indicate your wishes regarding resuscitation by checking the appropriate box. Make sure to review the options carefully.
- Sign and date the form at the designated area. Ensure that your signature is clear and legible.
- If required, have a witness sign the form. This person should not be related to you or be your healthcare provider.
- Keep a copy of the completed form for your records. It is also advisable to share copies with your healthcare provider and your designated representative.
After completing the form, ensure it is stored in a safe yet accessible location. Inform your family and healthcare team about your decision and where to find the document when needed.
Documents used along the form
In Texas, individuals often use several important documents alongside the Do Not Resuscitate (DNR) Order to ensure their healthcare wishes are respected. Each of these documents serves a specific purpose in managing medical care preferences, particularly in critical situations. Below is a list of commonly used forms that complement the DNR Order.
- Advance Directive: This document allows individuals to outline their preferences for medical treatment in situations where they cannot communicate their wishes. It can include instructions about life-sustaining treatments, organ donation, and appointing a healthcare agent.
- Boat Bill of Sale: This form is crucial for documenting the transfer of ownership of a watercraft in New York, ensuring that all transaction details are recorded. For more information, you can visit NY Templates.
- Medical Power of Attorney: This legal form designates a trusted person to make healthcare decisions on behalf of an individual if they become incapacitated. The appointed agent can make choices regarding treatments and interventions based on the individual's preferences.
- Physician Orders for Life-Sustaining Treatment (POLST): This is a medical order that translates a patient's preferences regarding life-sustaining treatments into actionable orders for healthcare providers. It is typically used for individuals with serious illnesses or those nearing the end of life.
- Living Will: A living will specifies an individual’s wishes regarding medical treatment in the event of terminal illness or irreversible condition. It typically addresses preferences for life-sustaining measures and other critical healthcare decisions.
- Do Not Intubate (DNI) Order: This order specifies that a patient does not wish to be placed on a ventilator if they cannot breathe on their own. It is often used in conjunction with a DNR order to clarify the level of intervention desired.
- Organ Donation Consent Form: This document expresses an individual’s wishes regarding organ donation after death. It ensures that healthcare providers and family members are aware of the individual’s desire to donate organs.
Utilizing these documents in conjunction with the Texas Do Not Resuscitate Order can provide a comprehensive approach to advance care planning. This ensures that healthcare providers and family members understand an individual's preferences during critical health situations.